Research
Research
Clinical needs
The idea for OxVPS came from our studies on clinical needs in visual perception screening after a brain injury.
In our first study, we interviewed 12 occupational therapists (OTs) and 13 orthoptists working in stroke services in the UK. We discussed visual perception issues after a stroke, the screening and referral process, and what makes screening challenging. From those interviews, we learned that clinicians seem to be less confident in screening for visual perception conditions like agnosia or reading than for visual neglect. A lack of training, time and standardised tests seemed to make it challenging for them to deliver the quality of care they would like to offer their patients.

We then checked if these experiences were common across the UK and Ireland. We also wanted to find out what the key barriers to screening for visual perception problems were. So, we ran a survey with 214 health care professionals involved in screening for visual perception difficulties after a stroke. Most of them were OTs or orthoptists. We learned that OTs screened for visual perception difficulties in 94% of services, with 75-100% of survivors being screened. However, many of the OTs screened for visual neglect only. They mostly relied on observations in function and self-report from stroke survivors: 94% of participants used these methods. Standardised screening tools and assessment batteries were only used by 56-58% of the OTs and orthoptists. A lot of people highlighted the lack of training on visual perception screening (20%) and the physical/cognitive condition of stroke survivors (19%) as the highest barriers to visual perception screening. They advised that a standardised screening tool for visual perception screening should be suitable for stroke survivors who struggle with communication (67%) and include management advice with the results (63%). The lack of training and overreliance on subjective screening methods might explain the current underdiagnosis of visual perceptual deficits in stroke survivors.
These studies motivated us to develop a screening tool that is quick, easy to learn, standardised, and suitable for stroke survivors with communication difficulties.
You can read more in our publications:
- Kathleen Vancleef, Michael J. Colwell, Olivia Hewitt & Nele Demeyere (2022) Current practice and challenges in screening for visual perception deficits after stroke: a qualitative study, Disability and Rehabilitation, 44:10, 2063-2072, DOI: 10.1080/09638288.2020.1824245
- Michael J. Colwell, Nele Demeyere & Kathleen Vancleef (2022) Visual perceptual deficit screening in stroke survivors: evaluation of current practice in the United Kingdom and Republic of Ireland, Disability and Rehabilitation, 44:22, 6620-6632, DOI: 10.1080/09638288.2021.1970246
Development
Once we knew what clinicians needed, we consulted vision scientists and reviewed theoretical models in visual neuropsychology to establish what the most important visual perception conditions were to screen for. To find out what the best tasks for each of these conditions were, we looked at paradigms used in visual neuroscience research, existing neuropsychological test batteries, and how well they differentiated between stroke survivors and healthy older volunteers. We came up with 15 different tasks for our prototype. We then asked for feedback from a large group of stroke survivors and older volunteers. Across 30 iterations, we received 620 comments and made improvements to the instructions, image sizes, fonts, etc. This resulted in OxVPS 1.0 which screens for 15 different conditions in only 10 tasks.
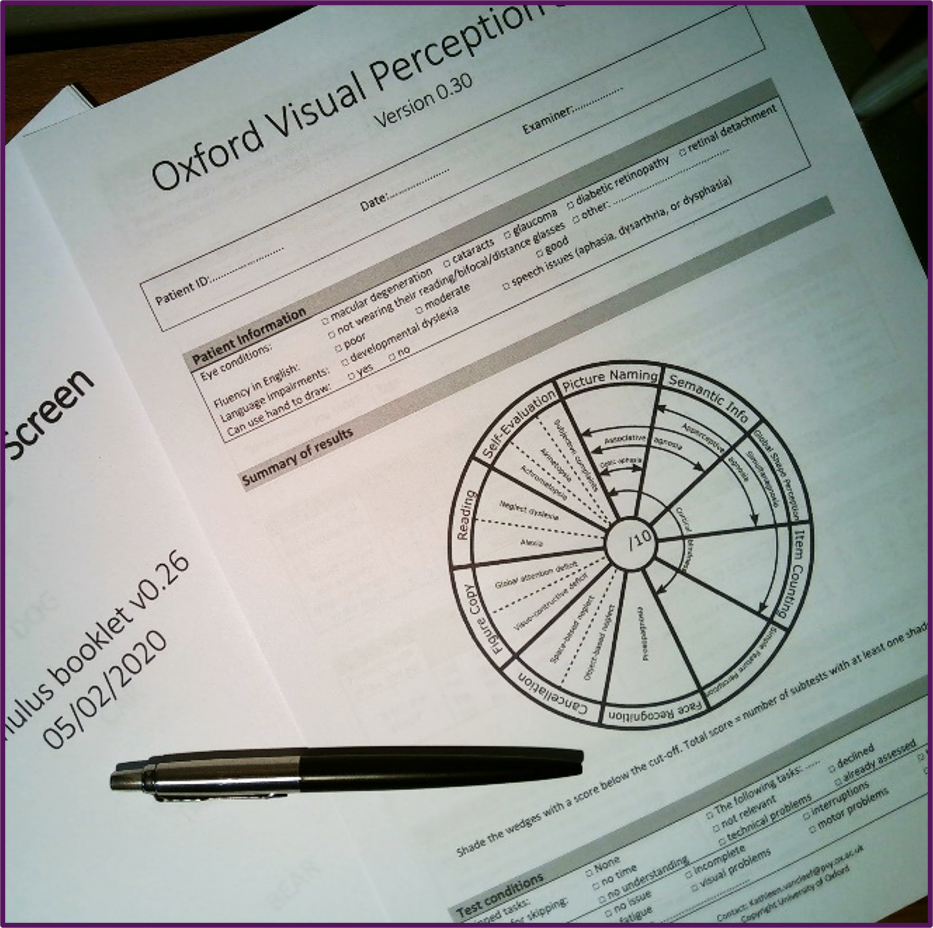
We then asked 80 healthy older volunteers to complete OxVPS 1.0 to establish it’s difficulty level. We were aiming for a test that was fairly easy for older people without a stroke and accessible for people with low vision. We learned that some tasks were still too difficult and some instructions were a bit ambiguous. To improve that, we made new stimuli for four out of the ten tasks and made minor changes (e.g. print size) to the other tasks. The new images of the four tasks were tested with another 125 healthy older volunteers. The end result became OxVPS 2.0.
You can read more in:
Vancleef K, Castellani R, Shorthose R, et al. The Oxford Visual Perception Screen: Development and normative data of a standardised assessment for visual perception difficulties. Clinical Rehabilitation. 2025;0(0). doi:10.1177/02692155251315606
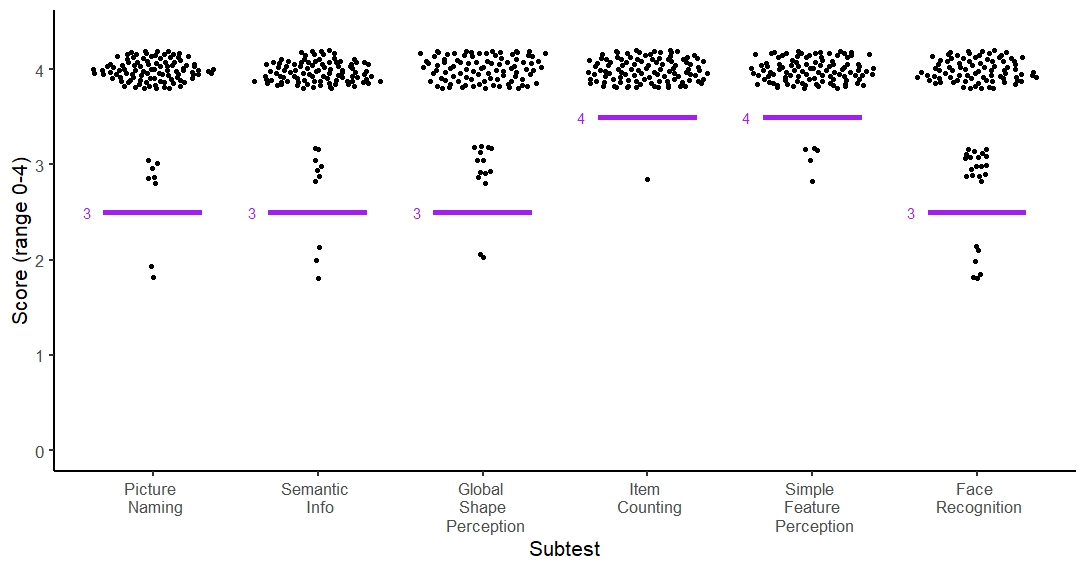
Normative data
Now we had final version of OxVPS that everyone was happy with, we could go out into the community again and ask healthy older volunteers to complete OxVPS. This is important because we need to establish what a ‘normal’ score on OxVPS is for people of different ages and from different backgrounds. We call this normative data. A ‘normal’ score is a score above our baseline score. We set the baseline or cut-off at a score that less than 5 percent of the healthy older volunteers have. For example, if most volunteers score at least 7 out of 10 and less than 5% of them gets a score below 7, than 7 is our baseline or cut-off score. So, we know that if a stroke survivor scores 6 out of 10 than that is very unusual and needs investigating further.
We recruited 107 healthy volunteers of similar ages as stroke survivors with many of them above 80 years old. They had not had a stroke or other neurological conditions. Just like stroke survivors, they could have other age-related conditions like cataract, macular degeneration, diabetes, or high blood pressure. We tried to find a representative sample of the population of stroke survivors. Some of our volunteers were retired professors, but others were factory workers. With their help, we could set baseline scores of each of the tasks of OxVPS.
You can read more in:
Vancleef K, Castellani R, Shorthose R, et al. The Oxford Visual Perception Screen: Development and normative data of a standardised assessment for visual perception difficulties. Clinical Rehabilitation. 2025;0(0). doi:10.1177/02692155251315606
Validation and diagnostic accuracy
Our next step was to test if OxVPS gives similar results to the current best practice test (that is accurate but time-consuming). In this study, stroke survivors on rehabilitation units in the North East and Oxfordshire were screened for visual perception difficulties with OxVPS and the Rivermead Perceptual Assessment Battery (RPAB, see picture below), the gold standard test for visual perception difficulties after stroke. By checking agreement in their scores on both tests we could evaluate diagnostic accuracy, sensitivity and specificity of OxVPS. In addition, we looked at the correlations between scores on both tests for convergent validity. The stroke survivors also complete a screening test for cognitive problems (the Montreal Cognitive Assessment or MoCA) and sensory vision issues like visual field defects, eye movement disorders or low visual acuity (with the Vision Screening Assessment or VISA). Comparing the result of OxVPS with these tests allowed us to check if the scores on OxVPS were influenced by cognitive or sensory vision problems a patient might have. This is called discriminant validity. If the stroke survivor gave permission, we video recorded the administration of OxVPS and another team member reviewed it to see if they would score it in the same way. This is called inter-rater reliability. In short, the stroke survivors completed 4 tasks (OxVPS, RPAB, MoCa, and VISA) and that allowed us to evaluate the accuracy of OxVPS from different angles.
The results from 62 stroke survivors who completed OxVPS and RPAB show that both tests are mostly in agreement with each other. We found excellent sensitivity of OxVPS: 87% of stroke survivors with visual perception problems were correctly identified. The specificity was good: OxVPS categorised 80% of the patients without such problems correctly.
The scores given by both team members, one who did the tasks with the stroke survivor and one who viewed the recording, were very similar. Our statistical analysis showed the difference was not more than 1 point on a scale from 0 to 10. We observed a correlation of 0.91 and intra class correlation of 0.95 which also indicated excellent inter-rater reliability. This means, that it does not matter who does the test, different therapists come to the same conclusion.
We also found a large correlation of 0.80 between stroke survivors’ score on OxVPS and RPAB and much lower correlations with MoCA (0.52) and VISA (0.41). This suggests that OxVPS indeed measures visual perception difficulties and less so cognitive or sensory vision impairments.
